Jane and Finch Medical Clinic

Jane and Finch Medical Clinic Approach to healthy life Life is movement and everyday life is full of activities and actions. So nobody can actually be insured against any injuries, traumas, illnesses or disorders. If you come with any disease it is really important to react quickly and do not let it turn into severe […]
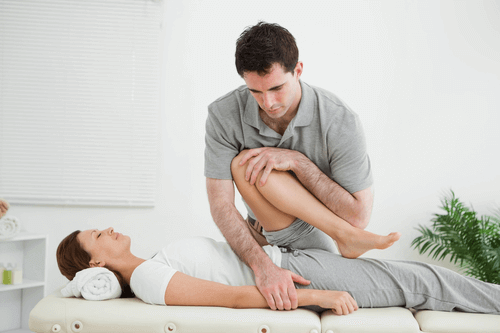
Physiotherapy clinics in North York

Physiotherapy clinics in North York Physiotherapy as a branch of medicine If you would like to get rid of the pain in your body, physiotherapy is an ideal way to do it. It is an area of medical treatment, which works for improvement of your health, wellness and quality of your life through therapy and […]
Acupuncture North York

Acupuncture North York If you feel pain and discomfort in your body or slackness of muscles and there is no medical way to help you or other health care options are not suitable for you, try acupuncture. It is needling treatment method which is used to cure a huge variety of health problems from the pain in […]
Car Accidents Can Cause Whiplash

Car Accidents Can Cause Whiplash Whiplash is a serious injury to the neck often experienced during rear end car accidents. Whiplash could also occur from side impacts and front collisions, too. Under normal driving conditions, the neck and body are moving in relative motion similar to the vehicle. When the car is struck from behind, […]
Best Massage Therapy in North York

Best Massage Therapy in North York Massage Therapy Did you have an injury, surgery or sport traumas? Do you suffer from pain, severe illnesses or stress? Try the treatment method such as ‘massage therapy’. The best massage North York is a mixture of therapy and relaxation which is an ideal treatment from different kinds of […]
How You Can Relieve Stress with Help from a Physiotherapist in North York
How You Can Relieve Stress with Help from a Physiotherapist in North York Stress is a part of our lives that we cannot completely ever eliminate. It is important to understand a low to moderate levels of stress can be beneficial to help keep us motivated and energized. However, when the levels continue to increase, […]
Why Physiotherapy Is Important After a Car Accident

Why Physiotherapy Is Important After a Car Accident When you are involved in a car accident, there are several factors at work, which can cause the body to sustain injuries. To being with, when you combine a moving vehicle with another moving vehicle or a stationary object, there are physical forces at work, most notably […]
The Difference between Chiropractors and Medical Doctors

The Difference between Chiropractors and Medical Doctors People have many misconceptions when it comes to chiropractic care and treatment. Some people believe visiting a chiropractor is only necessary when they experience a back injury or severe back pain. Other people fail to understand the extent of training chiropractors must complete and believe treatment options are […]
Injured at Work: What You Need to Know

Injured at Work: What You Need to Know According to the Government of Canada’s Labour Program, on average, one out of fifteen people are involved in an accident at work, which results in personal injuries. Employers do their best to help provide healthy and safe working environments. Unfortunately, it is impossible to plan for every […]
WSIB Approved Drug-Free Treatment Program

WSIB Approved Drug-Free Treatment Program Being injured, while on the job, is not often a pleasant experience. While most people might think injuries in the workplace only occur in construction, manufacturing, and other such labour intensive industries, they are mistaken. Even for people, who work in office, retail, restaurants, and other industries, they can be […]
